We asked one of the country’s top doctors a handful of critical questions that can help you navigate our strange medical system and live healthier and better.
You’ll learn: why medicine is failing us and what you can do about it, questions you must ask your doctor, a fascinating take on obesity, how to think about COVID, health topics you should and shouldn’t worry about, and more.
Quick updates:
This post is free to all subscribers.
Members get full access to our Premium content that goes out on Wednesday and Friday. Become a Member below.
If you pre-ordered my new book, Scarcity Brain, you can claim your free bonuses through this post. Pre-order a signed copy below.

The field of medicine, especially the annual check-up, is in a weird place.
It’s shifted from deep conversations about health and well-being between the doctor and patient, to a hurried checklist of numbers like scale weight, cholesterol, and blood pressure.
But by focusing only on numbers, we miss much more important aspects of health.
“Health is more than simply not dying; it is the painful, marvelous process of living.” That’s a line from Dr. Lucy McBride.
She’s a Harvard-trained MD who’s been practicing internal medicine for over 20 years in Washington D.C. She writes:
Health is more than the absence of disease. It is optimizing our medical outcomes, quality of life, and overall well-being. It’s about treating root causes and not just symptoms. It’s about marrying scientific data with our unique health conditions, connecting the dots between our medical issues and our everyday thoughts, feelings, and behaviors so that we’re armed with tools to live longer and better. It’s about empowering patients with nuanced guidance — plus structure and support as needed — to achieve their particular health goals. It’s about caring for our mental and physical health together.
During the pandemic, Lucy became a nationally recognized voice on the importance of addressing mental and physical health. She writes a fantastic Substack called Are You Okay? Sign up for it in the button below.
She has a book coming out with Simon & Schuster and a podcast called Beyond the Prescription. Her ideas have also been published in The Atlantic, the Washington Post, USA Today, and she’s appeared on NPR, CNN, MSNBC, and PBS NewsHour.
Which is all to say, she’s one of the top doctors in the country. And she’s asking bigger and more useful questions about health.
We asked her 11 questions that can improve anyone’s understanding of the medical system, how to navigate it, and smarter ways to think about health and living well.
P.S., Lucy ran a similar Q&A with me. Listen to or read my answers here.
1. In this post, you write: “The U.S. medical industrial complex is failing people. The wellness industry is fleecing people.” Can you explain your take on that?
Short answer
The way primary care doctors treat patients is changing in a way that isn’t ideal for long-term health.
Deeper answer
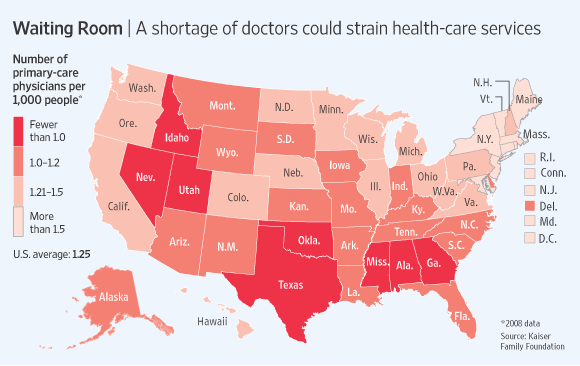
Absolutely, Michael. In the United States, we have two primary care physicians per 1,000 people. Approximately 80 million Americans don’t have a primary care doctor.
Because primary care doctors in the U.S. are in short supply, we often don’t have the necessary time and resources to address patients’ complex needs. Not to mention that the American medical system is geared toward damage control, not prevention of disease. Our system prioritizes testing, referring, and prescribing medications, not listening and learning from the patient’s story.
So, what happens when people don’t have a doctor or they don’t have enough time with their doctor to address all of their concerns? They go on the internet! The wellness industry steps in to fill that gap with oftentimes questionable recommendations—and profits off modern medicine’s failures to meet people’s needs.
Go deeper: I wrote an OpEd for The Hill about this.
2. In that same post, you also wrote, “To me, health is a process, not an outcome. Health is about awareness of our medical facts, acceptance of the things we cannot control, and agency over what we can change.” Can you unpack that?
Short answer
Figure out the aspects of your health you can change (for example, weight status) and those you can’t (e.g., genetic predisposition to heart disease). Then do what evidence shows will help you.
Deeper answer
Health isn’t fixed; it’s dynamic. Health is not defined by your test results at your checkup. It’s not about pleasing the doctor. It’s about the 364 days a year you’re not in the doctor’s office.
Why is agency so important? Because without it, we feel vulnerable.
We don’t know who to trust or what to do when we don’t feel well. In reality, people have more control over their health than they often think.
In my experience, people spend too much time trying to control the uncontrollable instead of putting their energy and resources into the areas where they have control.
My job is to help people carve out agency where they can.
Take, for example, my young patient with coronary artery disease who, in an effort to “take control” of his health, declines the appropriate prescription medications for his heart condition and instead takes handfuls of supplements every day based on what he reads online. His heart condition worsens. When he is able to accept that he has a genetic predisposition to heart disease (something he cannot undo) and when he is able to understand the data on treating coronary artery disease (and the absence of evidence on supplements) he is able to shift his focus and finally be in control of his health.
My goal is to help patients (and readers) understand what is fixed and what is dynamic in their health profile, to help them accept the parts they cannot change (due to genetics, environmental exposures, or behavioral issues), and then to help them identify — and work on — the areas they have control. Agency is the birthplace of health.
I recorded a short podcast to explain the concept of laddering up from awareness to acceptance to agency here!
3. I’ve had trouble finding a good general practitioner. During my annual physical exam, the doctor usually sees that I’m neither old nor obese, tells me I’m fine, and orders blood work. It’s a seven-second appointment, and I get no follow-up. What should I look for in a doctor? What questions should I ask her?
In short
These three questions will help you find a good doctor.
Go deeper
I am glad to hear that your tests and weight are normal, Michael, but as you know - health is about more than simply not dying! 😉
I’d look for a physician who listens well, who understands your goals and values, and who is interested in helping you improve your quality of life (not just quantity). I’d ask questions like this:
How do you conceptualize health? (Hint: I’d want to know that the doctor thinks beyond lab tests and biometric data and considers patients’ mental health, sleep, nutrition, exercise, and stress management/coping tools.)
What is your approach when a patient doesn’t feel well but the tests are normal? (Hint: I’d like to hear how he/she addresses invisible suffering such as fatigue, anxiety, insomnia, pain, stress.)
What is your approach to someone with mental health issues? (Hint: I’d like to hear that he/she is comfortable assessing these issues, is well versed on the benefits of behavioral modification, therapy, and stress management/coping tools— and has a good network of therapists and psychiatrists as needed.)
At the end of the day, you want your doctor to treat YOU—and not just your numbers.
4.When we spoke, you said something fascinating about obesity and how the medical-industrial complex is failing to treat it. You mentioned you see obesity as a symptom of something else. Can you explain what you mean by that?
In short
Lucy sees obesity as a symptom of underlying issues like poverty, emotional problems, etc.
Deeper answer
The medical establishment considers Obesity with a capital “O”—a disease, an endpoint. I see obesity differently—as a symptom of something else, a starting point, a reason to pull the curtain back on what’s really going on with my patient.
For some people, obesity is a symptom of poverty or lack of access to nutritious foods. For others, it’s a symptom of emotional eating or past trauma. When we medicalize emotional, behavioral or structural problems, we ignore root causes.
We also deprive patients of thinking broadly about solutions. When we help patients connect the dots between their relationship with food, their emotional health, their everyday habits, and the realities of their lives, we can create more nuanced pathways to improved health.
We need to treat the patient, not the number on the scale.
5. You wrote a post “Can Therapy Be Bad For You?” It cited a statistic that therapy doesn’t work for roughly 25 percent of patients. Why is that, and how can people get more out of therapy?
In short
People sometimes go to therapy to be heard and agreed with, but aren’t honest enough to be pushed.
Deeper answer
In my experience, one of the main reasons patients find therapy ineffectual is that human beings are generally more comfortable chewing on problems than challenging the way they think and behave. Talk is easy; change is hard. (For me, too!) Who doesn’t enjoy the cozy experience of venting our frustrations to a trusted friend, only to put ourselves back in the very place that brought us such ire?
The river is wide between our best intentions and the execution of change. Sometimes the water is too deep.
I’ve been in therapy myself where I haven’t disclosed the full extent of my issues in order not to be pushed. We do this as a way of protecting ourselves from discomfort. But in order for therapy to be effective, the patient has to be willing to be honest, vulnerable, and open to change.
6. When I have a random pain or symptom, I typically Google it. Which leads me to believe I have Stage 4 cancer. Luckily, I snap out of it after a minute or two. I know plenty of others who, like me, might be doing more harm than good Googling their symptoms. How do you recommend patients interact with Dr. Google?
In short
Make a doctor’s appointment.
Deeper answer
Ha! Dr. Google is always in! I recommend using Dr. Google with caution, remembering that it is unfiltered information—and that anyone can diagnose themselves with any disease on Google if they wanted to!
One of my patients was recently made very anxious from his adventures on medical Google. I told him that trying to diagnose himself on Google is like me trying to troubleshoot my broken-down car on the highway using the internet. I wouldn’t even try—I’d call AAA!
7. What’s something you’ve changed your mind on as a doctor in the last five years?
In short
We need more than numbers and data to improve a person’s well-being.
Deeper answer
That science and spirituality are not mutually exclusive. I am fascinated by (read: obsessed with) the re-emerging landscape of therapy-assisted psychedelic use for the treatment of anxiety, depression, PTSD and, ultimately, for healthy people who are looking to access their interiority and improve their health and wellbeing.
I have referred a number of my patients to some of the clinical trials. Stay tuned as I write more about this! To me, there is nothing more interesting than the intersection of consciousness and health.
8. What are a few quick ideas or tips you’ve learned from your podcast guests that have changed your behavior and the advice you give to patients?
In short
Everyone needs basically the same handful of things to be healthy.
Deeper answer
My podcast guests remind me (like my patients do) that everyone has a story, that everyone struggles, and that we all want the same things—to be loved, to be seen, to have purpose and meaning, to have human connections, and to be healthy and well.
Which is why my best advice to patients (and to myself) is often the simplest—to prioritize sleep, nutritious eating, regular movement, spending time in nature and with loved ones, and asking for help when needed. The rest is gravy!
9. What is something your patients worry too much about?
In short
COVID.
Longer answer
COVID! Of course everyone is entitled to their own tolerance for risk and their own threshold for worry, but I think that we did quite a lot of harm over the last 3+ years, stoking people’s fear even well after the widespread availability of vaccines and therapeutics.
So much of the messaging for 3+ years has been rooted in fear. Even in August 2023, with widespread population immunity due to the combination of vaccine-induced and infection-acquired immunity, people’s worry about COVID often seems out of proportion to the degree of actual risk.
I don’t blame them one bit! What people need is to understand how to frame risk, how to approach everyday decisions with another endemic virus woven into the fabric of everyday life.
Of course, COVID can do serious harm in high-risk patients, but it’s on par with the seasonal flu for most people—and it’s not going away. Instead of scaring people, medical messengers need to arm people with fact-based, realistic ways to balance the risk of infection with the risk of living in a state of perpetual vigilance. No one wants to get COVID, but health includes more than a negative COVID test.
10. And what are people not worried enough about?
In short
Booze and sleep.
Longer answer
Two things: The importance of sleep and the harms of alcohol.
Sleep is an essential ingredient in cognitive function, mental health, and overall functioning. Getting adequate rest is also important for metabolism and weight control. In our current “hustle” culture, I think we underestimate the value of a good rest!
Just because alcohol is legal and socially acceptable doesn’t mean it can’t do serious harm. From its potential negative effects on cardiovascular health, cognition, cancer risk, and mental health, sometimes I wonder how it is legal! I am not a prohibitionist. I love alcohol myself, but I think it’s easy to forget about its downsides.
11. Rapid fire:
What’s your favorite food when you’re not thinking about nutrition? Pop tarts. Strawberry-flavored, iced, toasted.
What’s your guilty pleasure? People Magazine
What is something most people don’t know about you? I was an au pair in Iceland for a summer during high school.
Where is an unexpected place you feel happiest? In a consignment store in DC called Ella Rue. It feels like home!
What would you do with $20 in a CVS that you HAD to spend? I’d buy a People magazine, a lip gloss, and a Diet Coke. HEAVEN!
What do you tell people when they ask you where you went to medical school? Do you do that weird thing where you say “oh, just this school right outside of Boston”? No. I tell people I went to Harvard Medical School. I’m proud of that. But I also tell people that most of what I’ve learned about medicine happened after I graduated from Harvard.
//
Thanks for reading. Have fun, don’t die, and consult a good doctor like Lucy, not Dr. Google.
-Michael
Sponsored by GORUCK
When I decided to accept sponsorships for this newsletter, GORUCK was a natural fit. Not only is the company's story included in The Comfort Crisis, but I've been using GORUCK's gear since the brand was founded. Seriously. They've been around ~12 years and I still regularly use a pack of theirs that is 11 years old. Their gear is made in the USA by former Special Forces soldiers. They make my favorite rucking setup: A Rucker 4.0 and Ruck Plate. Use discount code EASTER8 for 10% off anything from GORUCK.
Sponsored by Momentous
Momentous made me feel good about supplements again. Over 150 professional and collegiate sports teams and the US Military trust their products, thanks to the company’s rigorous science and testing. I don’t have the time or desire to cook perfectly balanced meals that give me all the necessary nutrients and protein I need (let’s face it, few of us do!). So I use their collagen in the morning; Recovery protein during hard workouts; essential multivitamin to cover my bases; creatine because it’s associated with all sorts of great things; and Fuel on my longest endurance workouts on 100+ degree days here in the desert (because Rule 2: Don’t die). And I also love (love!) that Momentous is researching and developing women-specific performance supplements. Use discount code EASTER for 15% off.
Sponsored by Maui Nui Venison
Axis Deer provides the healthiest meat on the planet. That's according to researchers at Utah State, who compared axis deer meat to beef and found that it contains 1 to 64 times more antioxidants, vitamins, minerals, and healthy fats. It also contains 53% more protein per calorie than beef. Here's a fascinating brief on the research. Equally important is that Maui Nui solves ethical considerations around meat. Axis Deer are an invasive species ravaging the Hawaiian island of Maui, and Maui Nui harvests the deer at night in a stress-free way, improving the ecosystem.
My picks: I like it and eat everything from Maui Nui, but the 90/10 Organ Blend is particularly great for people looking to get more micronutrients in their diet, and the Jerky Sticks are my go-to travel snack. Use discount code EASTER for 15% off.




Thanks for this fun collaboration, Michael!
Thanks Dr. McBride!